When hospitals go broke
Rural America has lost hundreds of hospitals and could soon lose hundreds more. Why is this happening?

Rural America has lost hundreds of hospitals and could soon lose hundreds more. Why is this happening? Here's everything you need to know:
How bad is the problem?
In many areas of the country, there's simply no nearby place to go to for a serious medical emergency or to give birth. More than 300 hospitals in rural areas have closed in recent decades, leaving tens of millions of Americans an hour or more away from the nearest trauma-care center. Over 2,000 rural hospitals remain, but more than half are operating at a financial loss, and 30 percent could close in the near future. Many have already cut vital services: Nearly 90 rural hospitals closed their obstetric units from 2015 to 2019, and by 2020 about half of all rural community hospitals offered no dedicated maternity care. When a small community hospital closes entirely, it can devastate the local economy and public health. A 2019 National Bureau of Economic Research study found that rural hospital closures increased nearby mortality rates for inpatients by up to 9 percent. "It is very dark, and I'm not exaggerating this," said Jeff Moses, an overwhelmed emergency room physician in Greenwood, Mississippi. "I just can't imagine what will happen to this community if this hospital closes."
What changed?
Several factors have conspired against rural hospitals, including an older and sicker population, people moving away, poverty, and the refusal of 10 Republican-led states to expand Medicaid. Hospitals that see fewer patients tend to have higher average costs. In urban areas, hospitals have been bought up by larger chains that cater to wealthier, well-insured patients to whom they can charge higher prices. Rural areas, though, tend to be older and poorer: Nearly a third of rural Americans are enrolled in Medicare, and a quarter of those under 65 use Medicaid. Forty states have now approved expanding Medicaid under 2010's Affordable Care Act, but three-quarters of the rural hospitals that have closed since 2010 have been in states that have not expanded their programs. Hospitals in these states have to absorb the cost of providing care to people who can't pay for it.
Subscribe to The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
What's the impact of closures?
The overall health in rural communities is worsening. Since 2010, the life expectancy for rural Americans has declined, and the gap between rural and urban mortality rates nearly tripled between 1999 and 2019. Cardiovascular disease accounts for much of that disparity: Rural adults have a 19 percent higher risk of heart failure than their urban counterparts. Rural Americans also have higher rates of obesity, hypertension, and use of drugs such as tobacco and methamphetamines. And while COVID deaths spiked in New York City and the Northeast in early 2020, the disease took a much greater toll on rural America after vaccination began in early 2021. Overall, the COVID death rate is 33 percent higher in rural areas than in urban ones.
Is the pandemic a factor?
Yes. Hospitals everywhere were put under strain by a flood of very sick patients, overcrowded emergency rooms, and staffing shortages. Since rural hospitals were struggling to recruit workers before the pandemic, they were hit particularly hard. A record 19 shuttered in 2020. But $15 billion in pandemic relief provided a vital cushion for those that stayed open: The following year, the number of rural closures dropped to two. That aid has largely ended, though.
What's the role of Medicaid expansion?
The Affordable Care Act offers federal funds to cover 90 percent of each state's cost of widening Medicaid eligibility to Americans just over the poverty line. (In 2023, people with incomes up to $20,120 qualify.) In states that have opted in, rural hospitals have higher operating margins and spend less on uncompensated care. Rural people in those states have also been seeking out preventive care more often, which may be keeping more out of emergency rooms. But 10 states, all with Republican-controlled legislatures, still haven't expanded Medicaid, despite evidence that their health-care systems stand to benefit financially. In Mississippi, the nation's poorest state, uncompensated care costs hospitals more than $600 million a year, and only a handful of hospitals are not losing money. A recent poll found that 80 percent of Mississippians — including 70 percent of Republicans — support Medicaid expansion, which Mississippi Hospital Association president Tim Moore called a "no-brainer." But Republican Gov. Tate Reeves continues to oppose what he calls "the expansion of Obamacare, welfare, and socialized medicine."
What else can be done?
The federal government's Rural Emergency Hospital program is now offering many struggling rural hospitals a trade-off: Reduce overnight inpatient stays in exchange for $3.2 million a year and a boost in Medicare payments. Participating hospitals would prioritize emergency and outpatient treatment, and transfer patients who need extended stays to bigger facilities. There is some resistance to the program because the delay created by transporting very sick patients can be hazardous. Still, many hospital officials say they have to do whatever is necessary to avoid a complete shutdown. "The math gets harder and harder," said Tom Reinhardt, the chief executive of a 10-bed hospital in Cascade, Idaho. "It would be irresponsible for me to not take this option to the board."
Maternal-care 'deserts'
Half of America's rural counties have no obstetric services, forcing 7 million women of childbearing age to travel long distances if they become pregnant. Maternal care is expensive, and often one of the first services an ailing hospital cuts. Fewer than half of rural pregnant women can now find needed levels of care within 30 miles, which is particularly dangerous for risky pregnancies. Counties with a high proportion of Black residents are more likely to lose obstetric services, and rural Black women's maternal death rate is triple that of their white counterparts. Christine Daniels of Jasper, Florida, had to drive 70 miles round-trip for her prenatal appointments in 2017. Medical workers missed signs of preeclampsia, from which Black women are more likely to suffer. She barely survived delivery, and her daughter sustained permanent brain damage. "I don't want nobody to go through what I had to go through," Daniels said. "It was scary. You feel alone."
This article was first published in the latest issue of The Week magazine. If you want to read more like it, you can try six risk-free issues of the magazine here.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
-
 Babies born using 3 people's DNA lack hereditary disease
Babies born using 3 people's DNA lack hereditary diseaseUnder the Radar The method could eliminate mutations for future generations
-
 A disproven medical theory could be guiding RFK Jr.'s health policy
A disproven medical theory could be guiding RFK Jr.'s health policyThe Explainer The miasma theory is one of the oldest medical beliefs in history
-
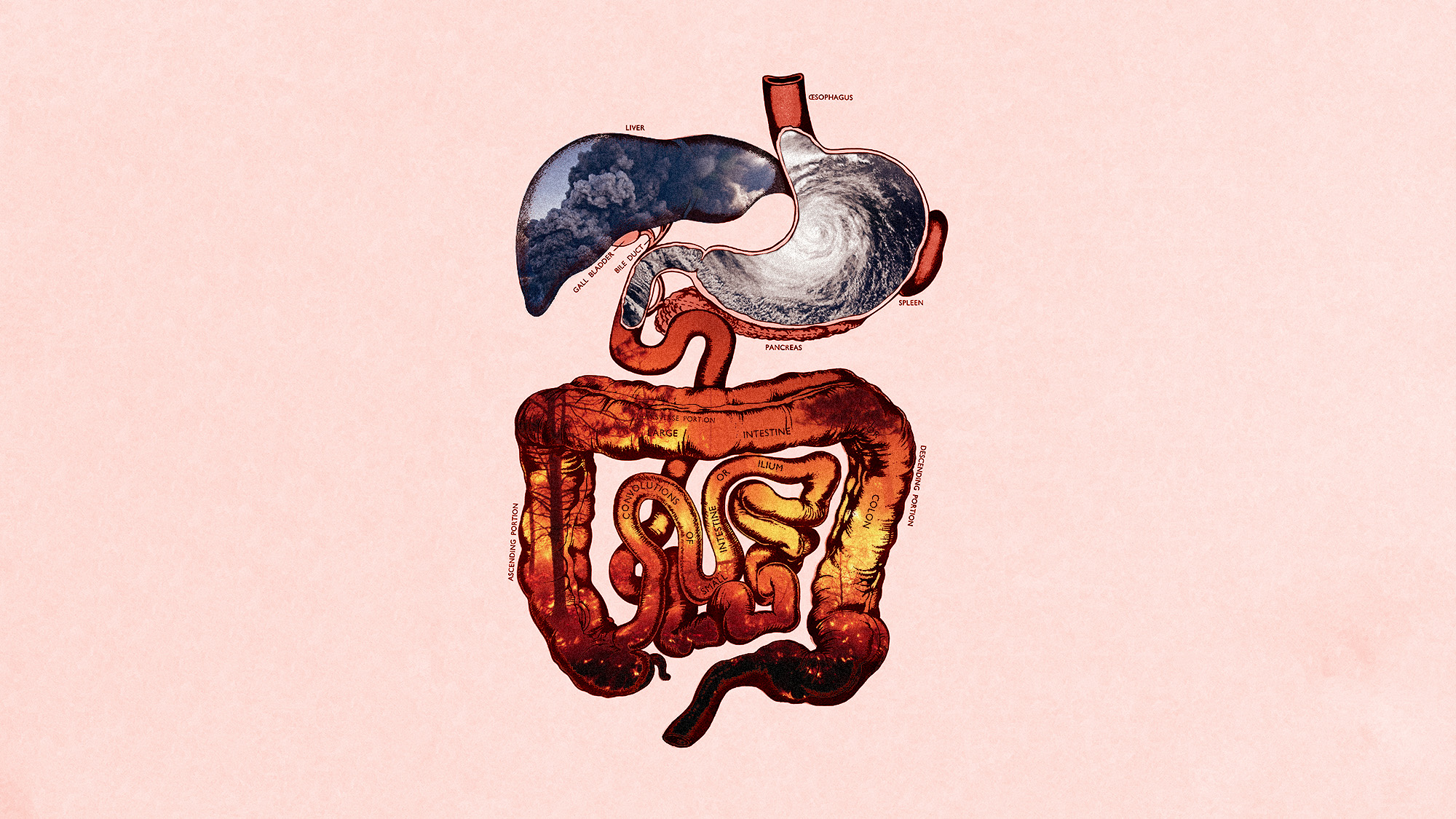 Climate change can impact our gut health
Climate change can impact our gut healthUnder the radar The gastrointestinal system is being gutted
-
 The marvelous powers of mucus
The marvelous powers of mucusThe Explainer It's snot just a pesky cold symptom
-
 'Wonder drug': the potential health benefits of creatine
'Wonder drug': the potential health benefits of creatineThe Explainer Popular fitness supplement shows promise in easing symptoms of everything from depression to menopause and could even help prevent Alzheimer's
-
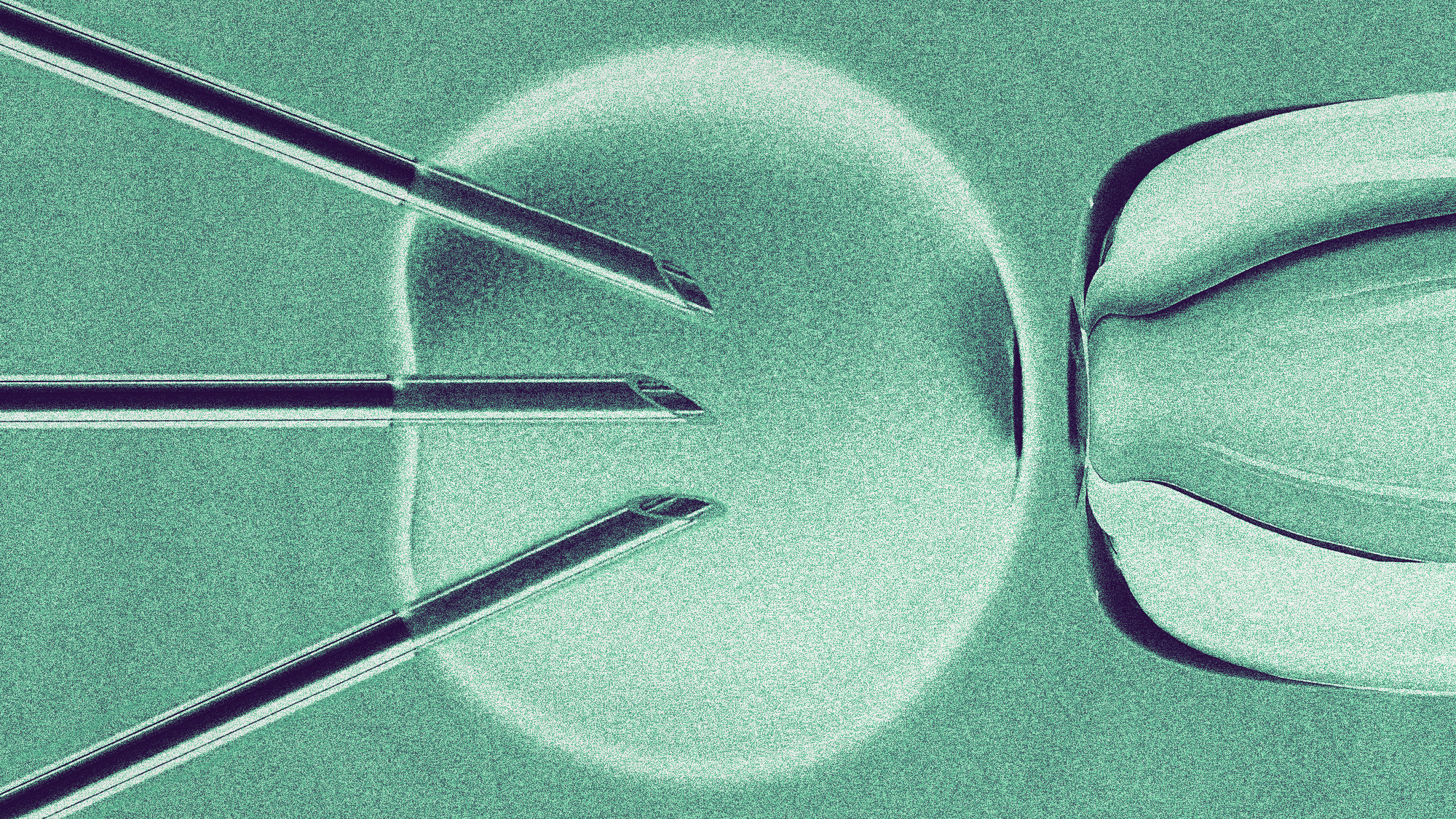
 Women need more pain management during gynecological procedures
Women need more pain management during gynecological proceduresUnder the radar Pain should no longer be ignored
-
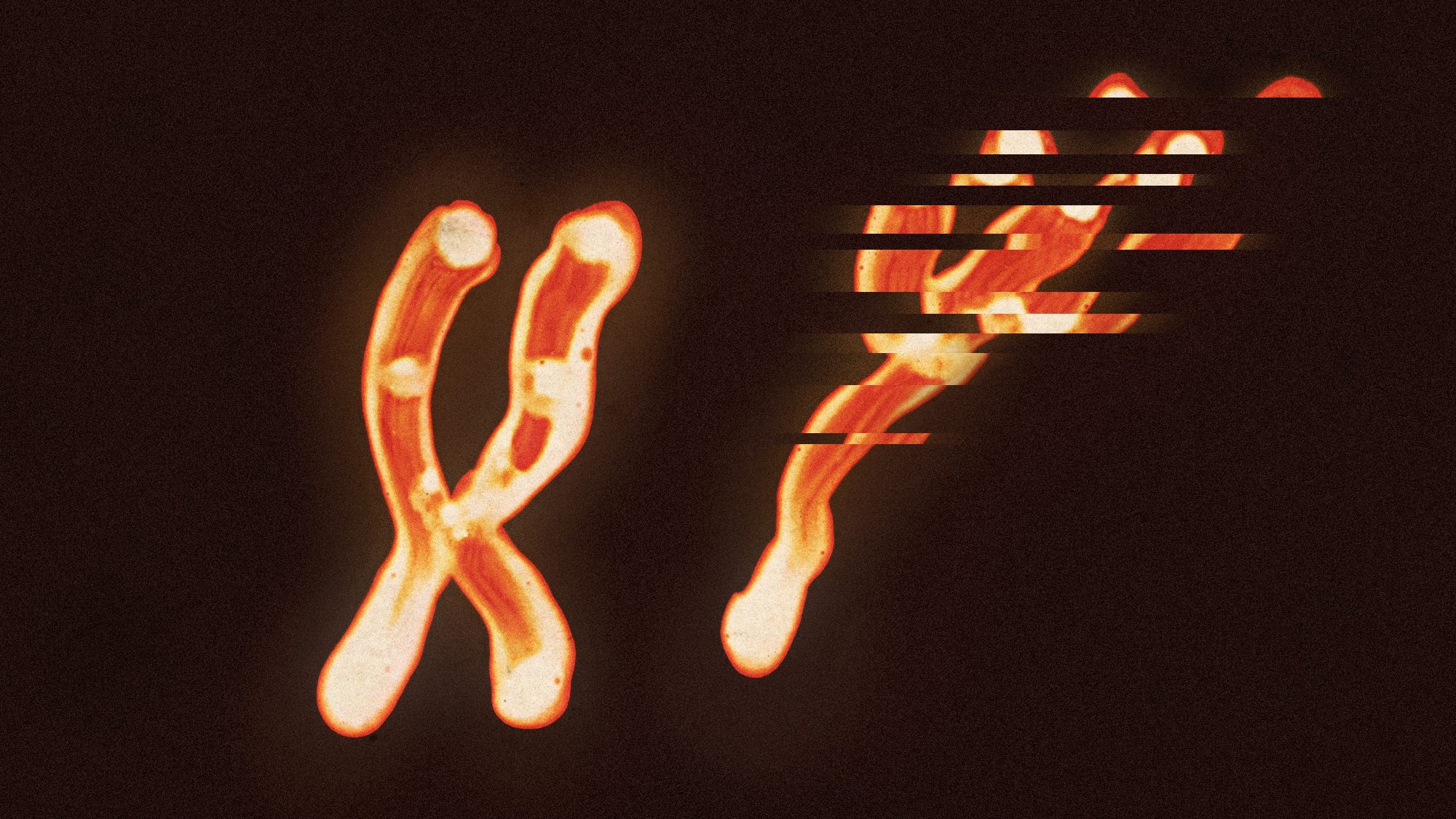 The Y chromosome degrades over time. And men's health is paying for it
The Y chromosome degrades over time. And men's health is paying for itUnder the radar The chromosome loss is linked to cancer and Alzheimer's
-
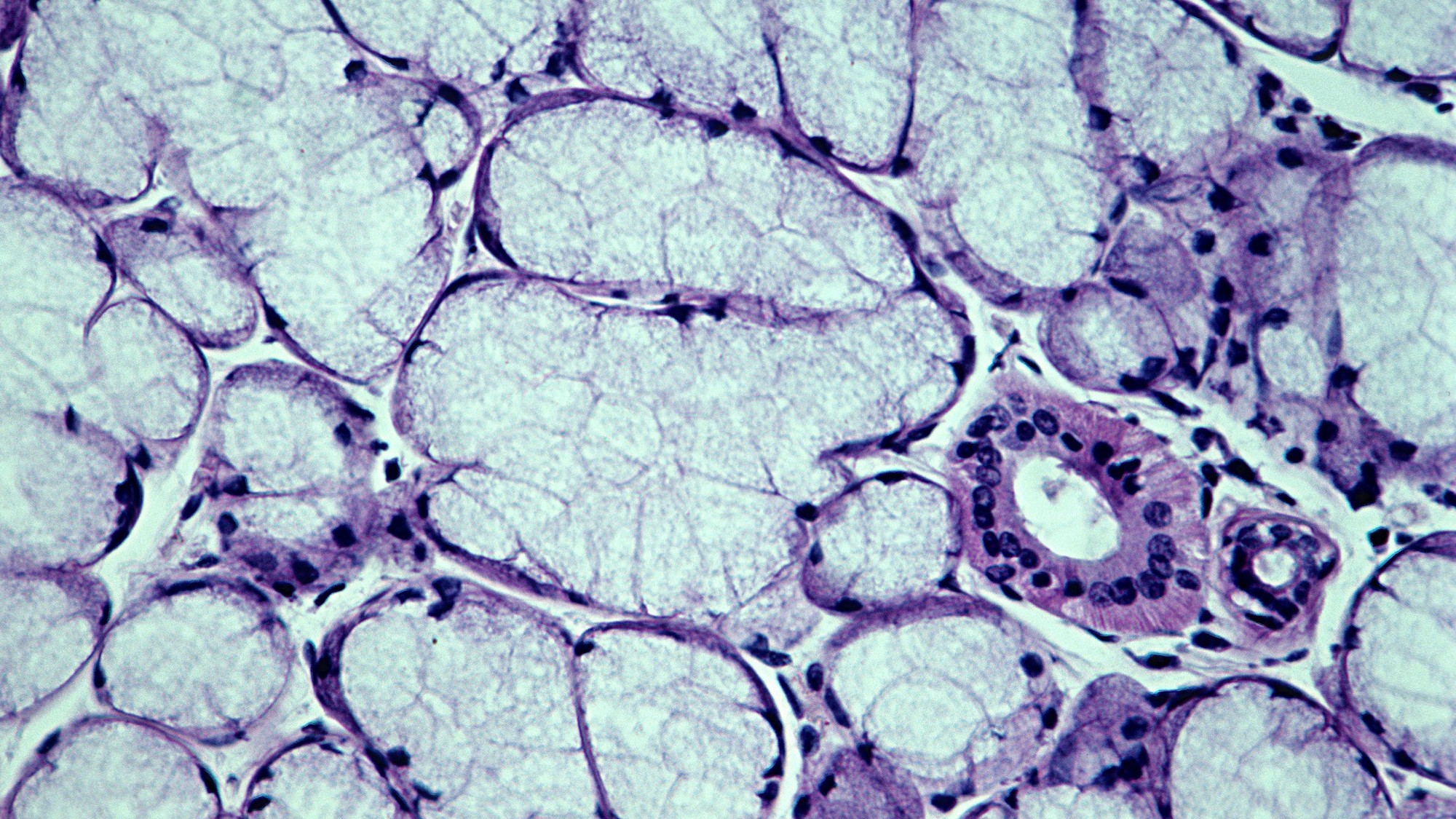
 A bacterial toxin could be contributing to the colorectal cancer rise in young people
A bacterial toxin could be contributing to the colorectal cancer rise in young peopleUnder the radar Most exposure occurs in childhood


